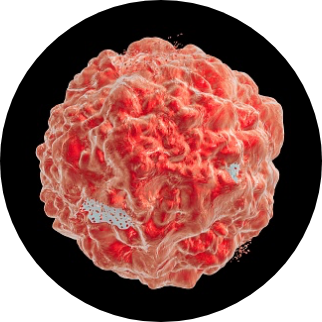
T cells are an essential type of white blood cell in the immune system.
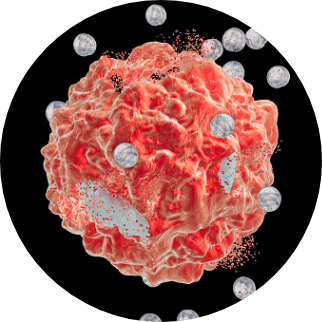
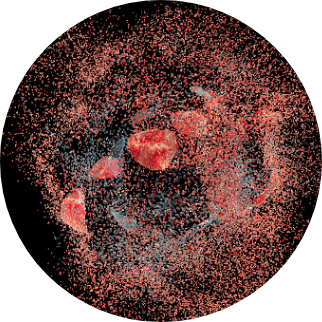
T cells are a population of different types of cells including so-called, alpha beta and gamma delta cells. They have the ability to eliminate tumors by using their T cell receptor (TCR) to identify cell surface markers known as cancer antigens, or tumor-associated antigens. Upon binding to an antigen, the TCR catalyzes a highly complex and broad signaling cascade that leads to T cell activation, proliferation, and tumor cell killing. In cancer patients, T cells frequently fail to either recognize or effectively engage cancer cells.