We are creating therapies using the natural biology of T cells to treat patients with solid tumors.
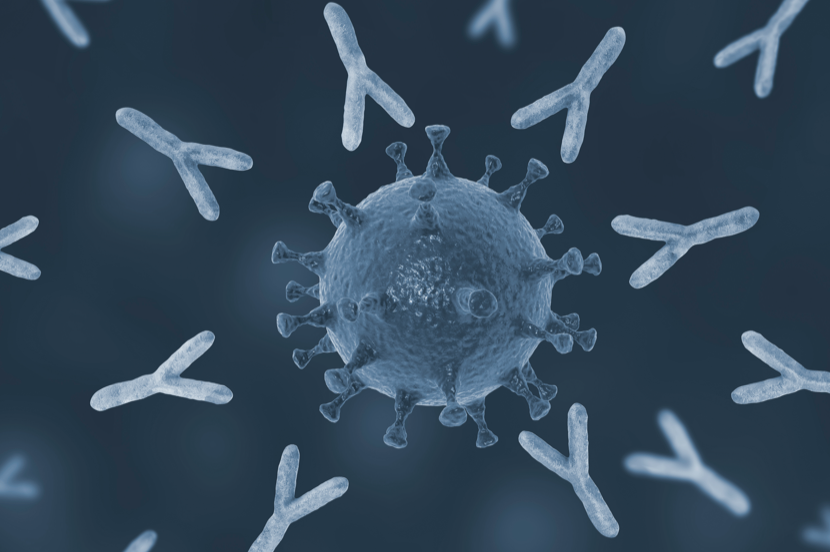
TAC, our proprietary T cell Antigen Coupler, is a multi-domain chimeric molecule that works directly with the T cell receptor (TCR) to help a T cell recognize and attack cancer cells. The use of an intracellular co-receptor sequence as one of its domains is completely unique to Triumvira. This non-gene edited strategy is designed to retain the T cell’s natural control and internal feedback mechanisms.
We believe TAC will become an essential tool for safely and effectively treating patients with liquid and solid malignancies. The initial target of our TAC-based programs is Claudin 18.2, a surface cancer antigen frequently over-expressed in a broad range of solid tumors.